An Introduction to Immunohistochemistry (IHC)



What is IHC?
Researchers are like detectives when searching for a new discovery in patient tissues. They use histological stains as clues for piecing together the story of what has happened in a tissue sample. This allows them to build a theory regarding what drives disease, and it then guides the next steps in translational research.
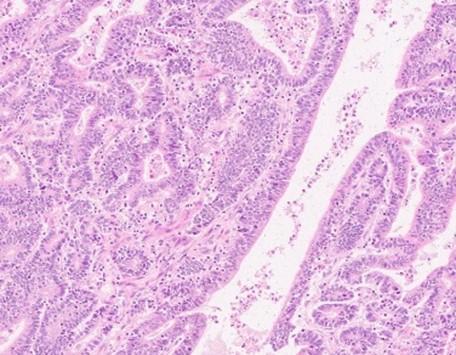
The first clue in the investigation comes from a routine or primary stain that uses two contrasting colors, bluish-purple (hematoxylin stains nuclei) and pink (eosin stains cytoplasm), defining structures and pattern changes in tissues (Figure 1a). This stain is called a Hematoxylin & Eosin or H&E stain. Investigation begins with the H&E-stained slide, and the pink and blue determine if further information is needed to clarify the findings.
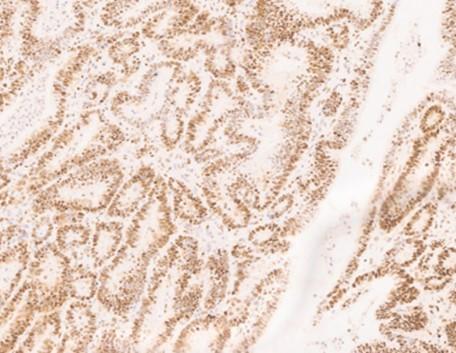
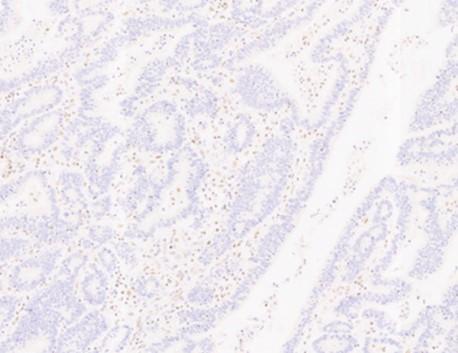
Figure 1. Bowel adenocarcinoma using H&E and IHC stains
IHC binding
Immunohistochemistry (IHC) is a specialized secondary staining technique, using chromogens, or colored precipitates, to clue investigators into an irregularity observed from the primary stain. IHC also utilizes hematoxylin as a counterstain to dye the tissue section. The hematoxylin serves to contrast the chromogen, and it also localizes to the nuclei for chromatin staining (Figures 1b & 1c). IHC is a standard laboratory test that is made possible due to the biological immune response in mammals. A subset of mammalian blood cells called lymphocytes can recognize matter in the body, not part of the host or self. Host cells express structures that signal to the lymphocytes that the cells belong to itself preventing the immune response from initiating their destruction.
Figure 2. B-cell Lymphocyte
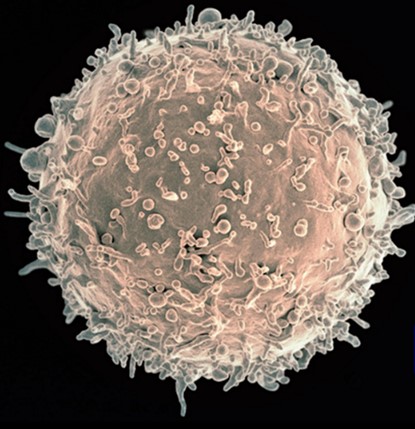
Image Credit: NIH NIAID1
B-cell lymphocytes (Figure 2) manufacture specialized proteins called antibodies which bind to the non-self-substance, marking it for destruction by other lymphocytic cells. IHC provides a focused look at the tissue to determine if protein expression is present or absent using antibodies.
What are antibodies?
Antibodies are specialized proteins called immunoglobulins that are generated by B-cells in response to foreign matter known as an antigen. Antigens are foreign substances that illicit an immune response or antibody production. They are Y-shaped immunoglobulin proteins that bind to antigens (Figure 3). The area at the end of each Y-arm recognizes and binds specifically to the antigen or target. These antibody-antigen-binding areas fit together precisely, like a key into a lock, latching the foreign material to the antibody. The antigen, or foreign material, is flagged for removal by other specialized cells. This is the body’s natural defense. IHC models this mechanism outside of the body on a tissue section mimicking the body’s immune system to find (Antibody) and flag targets (Antigen).
Figure 3. Antibody binding
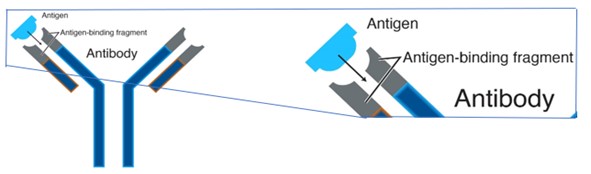
Image courtesy of National Human Genome Research Institute2
Antibody Creation
Generating high quality, specific, robust antibodies for research and discovery is a very rigorous process.
The relevant proteins that identify a particular tumor type are isolated, and these tiny protein fragments are used to inoculate a specialized lab animal to trigger their immune reaction. The animal's immune system will elicit an immune response, producing antibodies. Once there's a sufficient degree of these antibodies produced, the animal’s splenic cells are harvested, and the B-cells are isolated. The cells are held but cannot grow in culture.
To grow or proliferate in culture, the splenic B-cells must be introduced to a specialized malignant myeloma cell. The malignant characterization of the myeloma cell line makes it immortal, but it does not have the ability to produce antibodies. The combination of the B-cells with the myeloma cells generates a fusion of immortalized B-cells that can produce specific antibodies. This new cell is called a hybridoma, and it contains the best properties of both cell types. The hybridoma cell line can now grow in culture and produce the desired antibodies. These are the antibodies made to target proteins in diseased or pathological tissue sections.
Immunohistochemistry and Future Applications
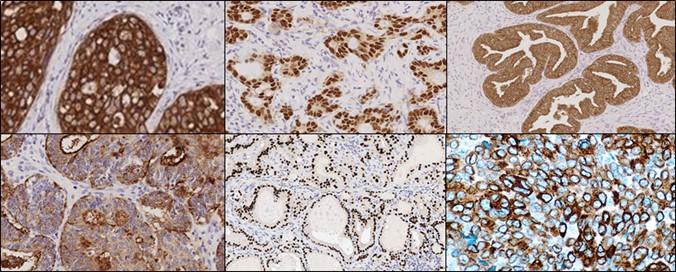
Cells secrete a wide variety of proteins. Abnormal changes in a cell affect protein expression: some proteins cease expression, others overexpress, and some modify into a new protein. Classification of these changes is based on the area from which they originated. For each type of cancer within a classification, research has determined a typical protein expression profile that can be detected and visualized using antibodies & IHC technique (Figure 4).
The staining generated by using antibodies and IHC generate data that may be used to move to the next stage of a research project that utilizes more innovative technologies like multiplexing, IHC staining with multiple antibodies on the same slide. By maximizing the amount of data from a single tissue section, researchers can uncover spatial relationships leading to a deeper understanding of the disease process and tumor microenvironment.
Figure 4. IHC protein expression profile
About the presenters

Denise has been with Leica Biosystems since 2015 and holds the role of Workflow Optimization Enablement Consultant, in Newcastle, UK. Prior to working for LBS she was a specialist biomedical scientist in Cellular Pathology for over 15 years working within NHS Pathology Services.

Jennifer Feldman began her career in the basement of the Life Sciences Building at the University of Memphis experimenting, in manual histology. After six years of research, Jennifer moved to South Florida and transitioned into the clinical setting as a histotechnologist at Holy Cross Hospital. It was here that Jennifer was able to train to quality and regulatory standards across clinical pathology. The need for automation and reproducibility in the clinical setting lead Jennifer into a field applications specialist role at Ventana Medical Systems where Jennifer was able to engage a broad range of internal and external customers supporting product development, launch, training, and sales. Today, Jennifer is the Innovation Partnerships Manager for Leica Biosystems. This team strives to bring new technology to researchers in the Life Sciences Space. Jennifer believes that we improve people’s lives by delivering technologies that matter.

April Schrank‐Hacker, Ed.D., Life Science Marketing Leader at Leica Biosystems, is a clinical laboratory specialist in Cytogenetics having over 30 years of experience in technology, research, innovation, and laboratory management. April earned her BS in Clinical Laboratory Sciences with a specialization in Cytogenetics from Thomas Jefferson University and is certified in cytogenetics through ASCP with the designation CG(ASCP) CM. Her Master’s degree was earned from the University of Pennsylvania in Organizational Dynamics (MSOD) with dual certifications in Organizational Development and Change Studies and Organizational Leadership. April earned her Doctoral degree in Organizational Leadership, where she was a Distinguished Research Fellowship scholar for her work on building high-performing leadership and teams in domains of chaos and complexity. She has coauthored over 30 peer-reviewed publications and posters.
Referencias
- National Institute of Allergy and Disease. Colorized scanning electron micrograph of a B cell from a human donor. National Institute of Health. 25 Aug 2016. Accessed 25 Feb 2021
https://www.flickr.com/photos/nihgov/29317535475 - Graham, BJ. National Genome Research Institute. Antibody. National Genome Research Institute. (n.d.). Accessed 25 Feb 2021.
https://www.genome.gov/genetics-glossary/Antibody
Related Content
El contenido de Leica Biosystems Knowledge Pathway está sujeto a las condiciones de uso del sitio web de Leica Biosystems, disponibles en: Aviso legal.. El contenido, incluidos los webinars o seminarios web, los recursos de formación y los materiales relacionados, está destinado a proporcionar información general sobre temas concretos de interés para los profesionales de la salud y no está destinado a ser, ni debe interpretarse como asesoramiento médico, normativo o jurídico. Los puntos de vista y opiniones expresados en cualquier contenido de terceros reflejan los puntos de vista y opiniones personales de los ponentes/autores y no representan ni reflejan necesariamente los puntos de vista ni opiniones de Leica Biosystems, sus empleados o sus agentes. Cualquier enlace incluido en el contenido que proporcione acceso a recursos o contenido de terceros se proporciona únicamente por comodidad.
Para el uso de cualquier producto, debe consultarse la documentación correspondiente del producto, incluidas las guías de información, los prospectos y los manuales de funcionamiento.
Copyright © 2024 Leica Biosystems division of Leica Microsystems, Inc. and its Leica Biosystems affiliates. All rights reserved. LEICA and the Leica Logo are registered trademarks of Leica Microsystems IR GmbH.