Fundamentals of Hematoxylin and Eosin Staining

For characterizing tissue, the use of H&E is by far preferred for viewing cellular and tissue structure detail. The variation of stain intensity is often driven by the slide reviewers' learning experience and what they are comfortable seeing. Because this stain demonstrates a broad range of cytoplasmic, nuclear, and extracellular matrix features, nearly all teaching texts use H&E images. We continue to use this simple and essential stain today, which has remained unchanged for over a century.
Learning Objectives
- Identify the four components of an H&E stain
- Describe the critical elements of developing an H&E staining protocol
- Define three characteristics of an optimal and suboptimal H&E stain
In this webinar, Cindy Sampias, JD CT(ASCP)HTL, Applications Technical Team Lead - Core Histology at Leica Biosystems, provides an overview and discusses the practical uses of the Hematoxylin and Eosin stains gleaned from over 30 years of laboratory experience in the field of histology.
During this presentation, Cindy provides insights and shares fundamental concepts about H&E staining, including the components, types, and “how-to” elements of developing protocols. Cindy shares “tips and tricks” with the audience on performing H&E staining optimizations and concludes by describing best practice examples of what to look for in optimal and suboptimal H&E stains.
For Research Use Only. Not for Use in Diagnostic Procedures.
Webinar Transcription
I am Cindy Sampias, applications technical lead for Leica, and today we're going to talk about the fundamentals of hematoxylin and eosin staining. One of the things that's been really fun with my job is being able to interact with customers as part of our cancer diagnostics process. One of the biggest questions I get is about H&E.
Overview
So why do we do it? In this particular lecture, we're going to be looking at not only why we do it, we're going to talk about the components. Is it better to stain by hand or on a platform? We're going to suggest protocols and then try to find the right balance between your colors, what our artifacts look like, and how can we troubleshoot some of those?
How do I fix these things? And of course at the very end, we'll talk about whatever questions you guys might have.
What Is It?
What is the H&E? Of course for our routine diagnosis, we're using this as our baseline. This is what’s getting us started. It really gives us a great opportunity to look at the cellular and tissue structure in detail. So whenever your slide reviewer is looking at a particular tumor type, whether it's benign or malignant, the stain intensity is one of the things that they're going to look at to determine just how bad things are.
In some cases, when you're talking about multiple chromosome anomalies in a nucleus, the more hematoxylin it picks up, is more DNA that's present in that cell. At the end of the day, most of the folks reviewing slides have their preferred coloration palette. Some people like it very, very pink. Others like it very, very blue. It just really depends on the end user and what they're looking for and of course, how they were trained initially.
We're going to talk about quite a bit of this today and ways to balance that stain out to get that side reviewer the exact coloration that they're needing for their diagnostics.
The Basic Components
We have 4 basic components. We have our hematoxylin, our differentiator, which of course is going to adjust the coloration of your hematoxylin, bluing, which is going to change the hematin from that reddish color to the blue color we're used to, and of course eosin which is our cytoplasmic stain.
Hematoxylin – An Overview
Hematoxylin is of course an acidophilic dye, which means it's acid loving. It's going to stain anything in your nucleus, which of course includes your DNA and your RNA.
There's a lot of different types of hematoxylin out there, and each one has a slightly different coloration appearance. Historically, we used to make all these things in our laboratories. You would have your hematoxylin powder and you'd mix it up. Now the challenge with that was making sure that if I made hematoxylin this week and you made hematoxylin next week, that we would get the nice balance there and our preparation techniques could influence exactly how those colors look.
Depending on who's making it, you're going to have a stronger intensity or a weaker intensity. The manufacturer commercially of the hematoxylin stain, whichever one you choose to use, has really made that quality nice and standardized. You don't see those variations based on preparation.
When you think about hematoxylin, oxidation is going to produce hematein, which is the actual dye in the stain. You can see this by looking at the top of your hematoxylin if you have it in a dish. You'll start to see it have almost a holographic appearance on top.
It reminds me of the sheen you see with E coli. That's the sign that your hematoxylin is being oxidized. One of the ways we stabilize our hematoxylin is by adding a mordant, and that gives the ability of the hematein to attach to an anion, something like iron, aluminum is another popular one that we use, and it helps stabilize it.
Hematoxylin – A Word About Mordants
Hematoxylins are usually classed by whichever mordant they're using. Like we said previously, the mordant is going to strengthen the positive ionic charge of the hematein. It's going to aid in the bonding of the hematein to the anionic tissue component, which of course is going to be your chromatin, your DNA, RNA.
Now because we're using different mordants that is going to influence the final color of the stain components. those changes are very, very subtle across the board. If you have a particular preference, you will notice the difference between Mayer’s hematoxylin, for example, and Harris hematoxylin.
The most common one that we use in routine histology is aluminum ammonium sulfate. This is going to cause a nuclei to stain red in color until we rinse it with a weakly-basic solution, i.e. our blueing solution. It's going to change it to the more familiar blue color that you're used to seeing.
Hematoxylin-Harris
Harris hematoxylin is the most commonly used alum hematoxylin, and it can be used for progressive staining and regressive staining of cytology specimens as well. It tends to provide a little bit clearer nuclear detail and one of the things you should know about it is that it can be best differentiated with the mild acid as opposed to using hydrochloric acid, which is a very strong acid.
Historically, we would use that. You would do one dip of the slide into your hydrochloric acid differentiator and you'd have to immediately get it into water. If you had it in there for two seconds, you could potentially completely decolorize the slide. Of course, we want to avoid that. The mild acids with your Harris hematoxylin is going to make that change a lot more subtle and give you as much control as you could possibly want in order to make sure you get just the right color that you're looking for. Harris hematoxylin is an alcohol-based stain.
Hematoxylin-Mayers Another one of our hemotoxins that we're very familiar with, of course, is Mayer’s hematoxylin. It’s another alum hematoxylin and it can be used both progressively and regressively, just like our Harris. It's also used as a nuclear counterstain for many special stains and IHC. It works really well in that scenario. It doesn't give you too much blue and it doesn't tend to stain other components of the cells.
When it's used as a counter stain, we want to see the nuclei and of course, then we're going to blue the slide without using any differentiator because we’re not concerned about removing any excess hematoxylin at this point. It is a water-based stain as well.
Hematoxylin-Gill’s
Gill’s hematoxylin is another one of what I consider to be the big three. It's an alum hematoxylin often used progressive or regressive and you can get it in lots of different concentrations of predominantly one, two, and three. It is typically used for cytology stains, but sometimes folks will use that in histology as well. It's made with water and ethylene glycol.
The oxidation of the stain is prevented over months because of this, and it just makes it more stable than Harris hematoxylin. Now the nature of Gill’s is that there is some extra nuclear staining that may occur. So this is where your differentiator can be really important for getting rid of that extra staining. And Mucin and even other adhesives on the slide can actually stain blue in the background. So you will see some more background stain than you would be experiencing with some of the other hemotoxins out there.
Hematoxylin - Others
There are quite a few other ones out there that use iron salts as a mordant, but they're usually in special stains. This is because they generally will demonstrate more tissue structures than the alum hematoxylin, so you can see things like myelin or elastin fibers.
One of the best known out there is Weigert’s, which we use in the Verhoff-Van Gieson stain or elastic stain.
Differentiator
Now the differentiator, we've talked about that just a little bit. What this is basically doing is allowing you to selectively remove stain from tissues to get the coloration that you're comfortable with.
When you're talking about hematoxylin, hydrochloric acid was used historically. Of course, it's a very rapid differentiator. Acetic acid or citric acid are the ones that are mild acids. Those are going to be for a much more controlled differentiation and those are the ones you're going to commonly see in laboratories.
While hydrochloric acid was the standard, it's really started to become more fashionable, I guess, to use milder acid because we are starting to use these things on platforms, automated staining instruments, that sort of thing. You're going to get a much gentler dye removal with that.
You know, automated staining has really brought some amazing opportunities into the laboratory for it increases in quality and production because we are able to do the same thing over and over again because you have those robotic arms on there. It makes it very easy for your techs to load rack; the instrument takes off, does its thing and now you've got your techs free to do other things in the laboratory.
This slide is an interesting one. This one has not had any differentiation at all. And if you notice there is a purple haze in the background and the tissue itself, this is tonsil, looks almost a little blurred. Now in this case I am using charge slides. So you can see in the lower right- and left-hand corner of the slide itself, there are little plus signs indicating that they are charged.
All that means is that the slides are going to have the tissue adhere much more strongly. Your differentiator would be used, and preferably a mild acid in this case, 30 seconds will get rid of this blue background for you. If you go up to a minute and now you're going to actually start being able to pull just a little bit of color out of the nuclei. If you have overstained it, you can see where you have a little bit more room to play if you want to pull out more color or not. Thirty seconds is going to be the minimum in order to get rid of all this blue background that we're seeing here on this charge slide.
Things like colon for example, which you can see in this image, depending on what you're looking at and who's looking at it, of course. You can notice that the goblet cells here are just… …do a progressive stain and that way you'll be able to capture the blue of this mucin in the goblet cells.
Bluing
Now let's take a look at bluing reagents. One of the most common ones out there is Scott's Tap Water. Certainly there are a wide variety of commercially available bluing agents out there that you can get to use in your laboratory, but they all function in the same way and that they are a mildly basic solution that's going to change that hematoxylin from the red to the traditional blue color that we're used to seeing microscopically.
Here's a great example of how bluing works, so if you take a look at this piece of tonsil here, you're seeing nice, delineated line. The top half of the slide hasn't been exposed to the bluing agent, but the bottom half has, and this is one of those things in your protocols you're going to see that the bluing is typically about a minute. Mostly that's to accommodate movement of the robotic arms on any of the stainers that are out there on the market.
The thing to know with that is I literally dipped this slide in and pulled it right back out. You can just see after one-to-two second exposure to the Scott’s Tap Water, it made a nice blue color here on the slide.
Eosin
Eosin is the most used counterstain. This is what's going to distinguish your connective tissue, your cytoplasm from your nuclei. It's generally going to be pink and there are different shades of pink depending on what type of tissue fiber it's staining.
So Eosin Y is the most common form and you can use it in both water as a base or alcohol as a base. Just a small amount of acetic acid added to it will also sharpen that detail in your eosin. It's kind of nice, especially if your eosin is weak. Just add a drop of acetic acid to it, and that should perk it right back up.
Eosin with phloxine is another common mixture that we'll see when it comes to eosin. There are a lot of folks that really enjoy how it enhances the reds on their H&Es. So when you're talking about cytology, there are other mixtures. In the case of eosin, we talk about EA50, EA65. These are going to add a little bit of light green, yellowish, and bismarck brown to the eosin. When you look at a cytology slide for example, a pap smear, you'll see the teals, blues, pinks, all of those shades of color and all of that's coming from your eosin.
Just adding those two extra guys is really what's going to make the difference. And of course the concentration of the eosin is determined by the designation of whether it's EA50 or EA65, which is going to have the most eosin Y added to it.
Eosin Differentiation
Now does eosin really need to be differentiated? Well, of course the right answer is yes, a graded alcohol, most commonly 95. Some folks will go as low as 70% alcohol and that's ideal to remove any of the excess eosin and that may be in the tissue. So what you'll be able to see is three different shades of pink. When you have too much erosion, just like with too much hematoxylin, if you don't get some of that excess out, then the whole thing is just going to be very bland, one color. Of course, that's not what we're looking for, right?
Higher grades of alcohol can also be used following eosin but remember, it's the water that's doing the differentiation for you. That's what's going to pull out that excess pink. If you go straight from eosin to 100, that's going to impact your coloration.
Staining by Hand or on a Platform?
What's better? Should we stain the stuff by hand, or should we use the platform? I can tell you as somebody who has done a lot of staining by hand over the years, the platform has just improved the quality and the quantity of work that we're able to get through in the laboratory.
For one thing you're staining is going to be very consistent. It's going to be reproducible. Of course, your technologists hands on time. They can go off and do the other things that may need to be done in the laboratory.
Now there are some concerns about potentially longer protocol times. Back in the day we used to say, I must have a 25-minute H&E stain. We were putting a focus, in my opinion, on the wrong thing. When you're looking at a platform, you can have 10-12 racks in process at the same time. Your protocol length maybe 50 minutes, but you're going to constantly have material coming off of your stainer. Whereas when we were doing things by hand back in the day, it was oftentimes a lot easier to have just one or two racks staining at the same time, so you didn't have 5 or 6 timers going off all over the place. This made it a lot easier. The other thing that's nice is you're much, much more able to follow your reagent management and make sure that your reagents are refreshed after a specified amount of time and a specified number of slides or runs going through them.
Protocols – Putting Them All Together
When we look at protocols, this is usually where folks struggle. Everybody has their own preference of what they want to see under the scope. What's the shortest possible time I can get? Turnaround time is huge and that's usually one of the things that kind of trips people up a little bit, because again, when you're talking about platforms, you're talking about having many things happening at the same time as opposed to just one or two racks at the same time.
We want to reduce those touch points, but then depending on what you're doing, how many touch points are there actually? Is the cost of doing it on a platform worth it? Depending on what you're doing, it may not be worth it. In most cases it is, but it depends on your laboratory and what your end game is.
Remember at the end of the day we have we want to have good quality and reproducible results. We want it to be cost effective and that's going to be the biggest concerns from most laboratories, the quality and overall cost.
Protocols – What Type?
What kind of protocols do we want to run? There are generally three different types. Progressive, which means there's no differentiation step. It goes hematoxylin, water, bluing, water, alcohol, eosin.
Now modified regressive or progressive depending on, you know if your glass is half empty, glass is half full person. There is a differentiation step utilized. However, the only purpose of that differentiation step is to get rid of the blue background. It's not going to impact your nuclear detail at all.
Regressive staining means we're going to overstain with our hematoxylin. Then we're going to use that acid to gently bring back and remove that background but also remove any excess dye from the nuclei.
Protocols – General Rule
General rules when you're looking at protocols, your H&E had that dewax set to get rid of the paraffin. Then you're going to hydrate it. That's usually done after going from xylene, to pure alcohol, to a graded alcohol, to water. Of course, in our hematoxylin differentiator bluing. Now we're going to start to introduce alcohol back in so we can do our eosin setup.
Then once it comes out of eosin, we're going to dehydrate it. Starting usually with a graded alcohol, going to pure alcohol. And then for our clearing step moving into xylene, toluene or some other aliphatic hydrocarbon solvent. And then we'll go to cover slipping.
The thing to remember with this suit is whatever you're using for your clearing, it’s often going to be the best reagent that you use in your cover slipper. Or if you're manually cover slipping, you want to make sure that it’s going to be compatible with whatever mounting media you choose to use.
The thing that's nice about this basic protocol is it's easy to reproduce and your reagents are going to be resilient enough to allow for a large number of slides to go through before your reagents need to be changed. That is so huge, especially if you're a laboratory where you're running 1000 slides every day. You want to know that your reagents and your setup is going to be able to tolerate that much workload.
Dewaxing and Hydrating
When we look at dewaxing and hydrating, xylene is going to be the most common solvent, at least in the United States we use it exclusively or some type of xylene substitute. There are lots of other things that you can use in its place. Some folks use toluene. Of course. We talked about xylene substitutes. There are things with citric oils in them like citrus, salt, limonene. Those are all different solvents. The thing is, you want to make sure that whatever you are using, you're going to be able to tolerate the slide volume that you're putting through the reagent. These things are all materials that are going to have to have special waste, just like xylene. Depending on where on you're at, those rules may vary slightly, but by the end of the day, they really are important to understand exactly what your local regulations are regarding waste of any of those solvents.
Once the paraffin has been removed during the dewaxing step, you can go into your alcohols and then your water and then move on for the rest of your staining. The water washes at the end of your graded alcohol is what's actually going to finish that rehydration, and it's getting it ready for the hematoxylin.
Hematoxylin – The Nuclear Stain
Depending on which hematoxylin you use, you want to make sure that there's plenty of time to get whatever coloration you're looking for. Once you've got to that sweet spot where you're like, this is what I like, now the slides are going to be rinsed. That's essentially going to stop the process and it's just going to remove any excess stain. Then if you want to differentiate your slide, you can certainly do that and then even control it even more by how long you leave it in that differentiator. Keep in mind, this is also going to include your background staining. You want to make sure that if you are going to use a differentiator, keep that in the back in your mind.
Any additives you may have added to your water bath, some folks use albumin. Some folks use sayon, or if you're using charged glass slides, all of those things are going to pick up your hematoxylin to some extent. So your differentiator here is going to be certainly something to consider while you're doing this. And of course. Once you're done with the differentiation, the water rinse is going to stop that now you're going to go into your bluing. You can use other buffers. Scott's Tap Water is one of the most common ones. It's very easy to make and it's not going to be something that's going to necessarily have as big of an impact on quality as, say, not being able to mix your own hematoxylin correctly. But it is going to change that reddish cast to the desired blue, as we saw in the previous slides.
Eosin and Beyond!
Before we add eosin of course, we want to make sure we use that 95% alcohol to get that sample ready to accept this alcohol-based dye. What's really fun about eosin is that you can adjust set coloration just with minor time changes. Eosin is amazing in that it will turn anything pink very, very quickly. If you've ever made hematoxylin from powder, you know that that powder is finer than confectioner sugar. If you get it on anything, you may not see it right away, but as soon as water hits it, it turns pink.
When I optimize slides for customers, I will do anything as low as 15 minutes, generally up to one minute, and I'll make those changes in 15 second increments. Any shorter than that, you're probably not going to get enough of a difference to be able to go, “Ah.” If you do it too long, then you're going to go from light pink to extraordinarily bright pink. That can be painful on the eyes if you're not used to seeing that.
The eosin of course is differentiated typically with the 95% ethanol. It's going to stop the staining process; some folks will use a 50 or 70%. It just depends on what you want to do. The more water in that alcohol following, the eosin is going to pull out more of that pink color for you. If you're tending to over stain with your eosin, you can use a 50 percent, 70%. Those will pull out the eosin because they have such high water content.
Normally, we would do 95% of ethanol and then you're going to go from that to a pure alcohol and then your clearing so that you can get that slide coverslipped and ready to view.
A Word About Solvents
Let's talk a little bit about solvents. There's a lot of different choices out there for your dewaxing and dehydrating. Here in the US, we tend to use xylene. That's our most common, but that's not to say there's certainly aren't others out there that are worth using.
Some places like to use taliouine and then of course we have then wide variety of xylate substitutes that are out there. The thing to know about xylene substitutes. They’re going to be a lot less tolerant to water, so if you have ambient humidity, you're going to start to see decreases in quality.
One of the things you may notice is if there is water in your clearent and it goes to cover slip, in a few days you might notice a pink haze shifting across your slide. That's the water that was captured in that clearent pulling the eosin out and you're starting to see that drift across the slide.
With any of these substitutes, they are going to have the same waste disposal requirements. Keep in mind you are getting a product that you can't use as long, you're going to have to dispose of it the same way and that can be extremely costly. There may not be a compatible mounting media out there for that solvent. Citrus based solvents, which are personally my least favorite. Because they're so aromatic, they can actually cause reagent sensitivities in folks. I've seen this in laboratories where after working with them for a few months, folks will start to get migraines around things that they wouldn't have otherwise been bothered by, which is to me, it's kind of sad. I like the idea of what's behind it, but at the end of the day, it's not necessarily the best fit. That doesn't mean don't use it, that's just been my experience.
Foundation Protocol
There are a lot of different protocols out there. I have my personal preference. I try to keep it very, very simple. You want to make sure that your slides are dry so you can always add an oven step if you want. 15 minutes at 60° is fine. We'll talk a little bit about some of the artifacts that you can see and what causes them. One of those things can potentially be that oven step, but you can see here you have xylene, xylene, 100 ethanol, 100 ethanol, 95 ethanol, then we go right into a wash station or hematoxylin and then all the way back out and the back end is essentially the reverse of the front end. 95 ethanol, 100 ethanol, 100, ethanol, xylene, xylene out.
Some of these steps I do keep as exact. The reason for that is you don't want your hematoxylin to potentially be in there longer than four minutes if four minutes is your sweet spot for your color. Same thing is true for your differentiator, this is a very key component.
Bluing. Most folks just make it exact because it's a staining component. It's not nearly as critical as having your differentiator or hematoxylin. When you get to eosin, you want that to be exact. We also want that first 95 and that first 100 following it to be exact because the 95 has water in it.
If you have it in there for a minute and your standard builds in tolerances to allow racks to continuously be moving through, what will happen is it could stay in there longer, which means it's going to pull more eosin out. Now, because your rack coming out of that 95 is going to go into that first 100% ethanol there is going to be some water carried over just because the slides aren't coming out of that 95 dry. I make that step generally exact as well for the same reason to reduce the potential for any bleeding of the eosin.
Balance is Key
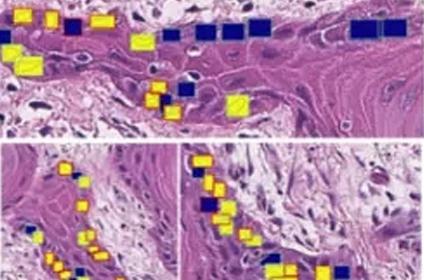
Balance is important. We want to get the color quality that we'd like, but we also want to make sure that we get the balance of the blue and the pink. What's interesting is you can see in this slide the difference, two minutes of hematoxylin for the sample on the left versus four minutes for the sample on the right.
I can also have fun with this by playing with my eosin. By increasing my eosin time, everything will be a little bit darker, but I can play with my two hematoxylin and eosin colors because they do play off of each other. What will happen is if your pink is really bright, it's naturally going to make the blue of your nuclei seem a little bit lighter and the other way around. If your nuclei are super dark, your eosin may look a lot lighter in color underneath scope and it's just because of the balance.
If you want your eosin to be brighter, maybe dialing back the nuclear stain just a smidge, and by that I mean 30 seconds to a minute might make all the difference that you need to get that eosin to the brightness that you like without compromising your nuclear detail.
Protocols
The other thing that's kind of fun to think about is when you're looking at your stain quality, looking at things grossly is not always your best friend. I always recommend folks review their slides under the scope before they decide whether the intensity is appropriate. As you can see here, I've got a nice piece of tonsil followed by a piece of lung and then a piece of fatty breast tissue. Notice that those all look wildly different when it comes to how much hematoxylin was picked up. A lot of that is going to be due to the tonsil being highly cellular with very little cytoplasm. Your lung tissue has a lot of open spaces in it, so it makes it look like pink is hardly there. When you look at the fatty breasts, it's even more difficult to see any nuclei at all. Those are all stained at the exact same protocol, the exact same hematoxylin and eosin stainings.
However, the cellular components themselves are driving the differences in gross appearance. We want to be thoughtful of that. If we are deciding about whether we like something, if we think it's the right colors or not, always go microscopically because grossly, it can throw you off.
Do I need a Control Slide?
Should I run a control slide? I always recommend that you do. I'm a big fan of sausage blocks. Those are analogous to microarrays, except they're way cheaper to make. I like to use things like tonsil. Tonsil is great because it's highly cellular, very low cytoplasm, so you're really going to get the nice intense blue. Colon is fabulous. It has a lot of cytoplasm. You can also get muscle fibers and some fat connected to that as well. You’re going to have a range of cell types to be able to look at microscopically.
Skin is nice. A dermatologist oftentimes will have a particular color scheme that they're going for. If that's what you're studying and your lab, whoever is going to be reviewing your slides, these are the three things that are going to give you an idea in one simple slide of how your stain is going to work across a variety of different sample types.
I strongly recommend using this as a control. Is it absolutely necessary to use these 3 skin types? No, feel free to make something a sausage block. Make it your own. If you're predominantly doing liver and stomach, then make your control consistent with that. You'll know exactly what you should be expecting.
Optimization
Optimization is a question that I hear about a lot. How do I perform it? Normally when I'm doing optimization for my customers, I will take a look at their slides, what they currently have and I'll ask them, “do you like this?” Sometimes they say “Yep,” sometimes they say “No.” Then I have to unpack exactly what it is that they don't like about it.
I’ll pick breast, colon, skin, tonsil and uterus because that covers a nice wide variety of different sample types and different nuclear to cytoplasmic configurations. I will also then grab my preferred stain. I will stain my sample slide with what they already have and then I will tweak it with whatever stains I'm moving in to work with the customer. I will use that and try to match them.
If the customer is like “I have no idea, I just want something better than this,” I will usually sit down and ask them, “What does that mean for you?” If they want it to be more blue, if they want it to be more pink, depending on what direction they want to go with it, I'm very easily able to help them adjust their stain to get exactly what they're looking for color-wise.
Typically when I'm doing an optimization, I will increase or decrease my hematoxylin by 30 seconds and my eosin by 15 seconds. If you really want to get nuanced about it, you can even go further and adjust your time of your differentiator. Adjusting it from one minute to a minute and 30 seconds is going to make your hematoxylin just a little bit less pale. For simplicity’s sake, we'll go with just increasing or decreasing hematoxylin and then increasing and decreasing your eosin.
When I am doing this, I will have several different sets of slides. I will put my different stain variations in a little table, and I assign randomization codes. Part of the reason I do that is because there's a lot of folks that think they know what four minutes in hematoxylin looks like on every possible hematoxylin out there. That’s not the case.
To get them away from trying to assign numbers to things, what I like to do is just give them slides and say, “tell me what you like.” By not giving them any other information, except “here's your slides, tell me what you think,” that forces them to go strictly on what they like to see and not necessarily adding in any other, “Is my hematoxylin long enough? Do I want my eosin to be shorter?” whatever any of those extra variables will be, it makes it very simple.
One of the challenges I will tell you that I see from time to time is water quality. Water quality will make four minutes in hematoxylin look very different depending on what the problem is with your water quality. This is why when I do my optimization, I give them randomization codes and I have them write down what they like and what they don't like and then we go back from there and adjust it. What's great is it makes it so much less stressful when you're working with whoever is reviewing the slides directly and it just simplifies it for them. It makes it so much easier for you.
Artifacts
Let’s talk a little bit about how these things are supposed to look under the microscope. If you look at this slide, you'll see a nice piece of normal lymph node. What's interesting about this one is it doesn't look like there's very much eosin in it at all. Keep in mind that our nuclear-to-cytoplasmic ratio is very different here than what we would see on a well-differentiated squamous cell with a tiny nucleus and lots of cytoplasm.
You can also see the nuclei are very clear. We have some stromal cells in here. Of course, some red blood cells. Everything looks nice and crisp.
Normal Placenta
This is a nice piece of placenta. As you can see here, we have some variation in our eosins. We do have a lot more cytoplasm here. The nuclei are going to take a back seat a little bit to the pink. You'll see that we again have different colors of the pink in here. It's really showcasing that cytoplasmic detail.
Balancing the Scales
How do we get everything balanced? Look at this slide here. We have a nice section of lymphocytes on the top with muscle fibers underneath. This is again where that balance is very important and why you want to make sure that your control slides represent a variety of tissues.
At the top half of the slides, it looks like we only stained it with hematoxylin, that's because. There really isn't any cytoplasm around your lymphocytes. Those are very, very small cells with almost no cytoplasm. As we go down to the muscle fibers, though, you'll notice that cytoplasm is the predominant component here. So even though we still have periodic nuclei, of course, within the cells, you can see that we have.
The colors are the same between the lymphocytes, coloration of the nuclei and the nuclei down here in the muscle fibers. Notice how rich that pink is. With this particular sample, we would be able to dim the light a little bit, and you'd be able to see the refractile nature of those muscle fibers.
This is one of those things where it's important to understand just how that balance can make a difference depending on how many nuclei you have versus how much cytoplasm.
Adenocarcinoma of the Colon
This one is interesting. This is an adenocarcinoma of the colon. You can see where we have some normal nuclei and then we get right into the abnormal ones. Now malignant nuclei are very irregular in shape and you can notice that because of the different amount of DNA that's in these. You're going to see some different coloration as you go through all those nuclei, but for foundation we have some pink in here with some red blood cells. We have some stroma, and of course we have some lymphocytes around here.
That's one of the things that you can always use as a guidepost. Look at the normal nuclei that are in your piece of tissue. And you can see a strong difference between those and your malignant nuclei. And it's profound depending on what you're looking at.
Tonsil
This is a piece of tonsil. This one is incredibly pink. In this case, the preference of the reviewer was to have a much lighter, nuclear stain and really enhance the eosin in the background. I don't care for this balance, but I'm not the one that's reviewing the slide, so this is certainly not wrong by any means, but in my opinion it's not ideal.
This is where you want to make sure that your side reviewer has the most say and what they want to see microscopically.
Water Quality
Let's talk about water quality. You can see slide A and slide B. Slide A and slide B are from the same block, but they look very different. Water quality is often an issue I see in the field and on one side could be very acidic. The other side could be very basic. When your water is very acidic, that's not going to negatively impact your hematoxylin, because essentially, you're taking acid water and putting it into an acid dye. By keeping that pH appropriate in your hematoxylin, you're not going to deplete it.
When you come out of Hematoxylin now and you go into that wash following it, that acid water is going to decolorize your slide a little bit before you put it in your differentiator. Every subsequent water wash is going to pull more and more hematoxylin out.
If the water is basic, what's going to happen is you have a higher pH liquid carrying over into your hematoxylin. That's going to weaken your hematoxylin and it's not going to allow overtime to continue the nice coloration that you would be used to if you had stable water. Your first slides of the day may look great. As the day progresses and more of the alkaline water gets added into your hematoxylin just by normal carryover, you're going to start to see your hematoxylin lighten up a little bit. This is one of those things that if you're getting inconsistent staining and you're not sure why, the pet store and water testing strips is a great way to just test your water and kind of a ballpark of where you're at.
This doesn't have to be dead exact 7.1 measurements. We're talking, “Is it 7.5? Is it 9?” That's what's going to help you with this particular artifact is to make sure that your water is stable. That will give you stable staining overall.
Nuclear Bubbling
When folks bake their slides, which I completely agree is great. It helps you dry your slide quickly. It melts that paraffin a little bit. When it goes into that first xylene, you have a nice warm slide that that wax is going to come out very easily.
The problem is some folks try to do too much with the heat. Putting it in a hot oven, and there's a lot of water underneath, is going to vaporize that water through the nuclei, which are proteins and it's going to create nuclear artifacts like you see here, which we call soap bubbles.
When you're looking at a prostate tumor, the downside to this is that not only are these nuclei very fragile, but nuclear changes like that can also be indicative of some malignancy, such as thyroid cancer. One of the trademarks is to have a nuclear hole in it like you see here. The downside is if your patient has a normal thyroid, but it goes through temperatures like this and ends up causing nuclear bubbling, it can create a false positive. You'll be misinterpreting what would normally be considered standard diagnostic criteria for a particular tumor.
You want to bake with care and there is no going back from this once you've gotten their bubbles, there's no way to fix this, unfortunately.
Formalin Salts
Some of the things that we use when we're doing our stains can leave pigment behind. Formalin pigment is one of the big things. You can see some here. If you're using good quality reagents, it's not as much of an issue. Some of the poor-quality ones, some of the poor-quality hematoxylins, if they're not filtered, you can start to see some of these pigments in here.
Your fixatives can also impact that. Back in the day, we used to use anchors, which was a combination of mercuric chloride and potassium dichromate. Often, we would see this type of particulate. Don't let those things dissuade you from making your diagnosis. These things can unfortunately show up and they have in some cases tripped folks up. Just be aware that they are out there.
Caudery Artifact
Caudery artifact is another issue that we see. You'll notice how one end is kind of blackened and kind of fried, and all the nuclear detail there is gone. This is again something that we'll see during processing. One of the things that can also cause that is if you take your biopsies out, and you like to use sponges or wraps, make sure that you make those sponges and wraps wet with whatever your fixative is.
Never put a sample onto dry paper towel and then try to wrap it up in that little piece of wrap and put it in a cassette. That's going to pull all the liquid out of your sample and you'll start to see some of these edges like this. This is also can be caused when the sample is collected. If you're using a caudery iron to collect your sample, this will also happen. Just keep that in mind as you are working through your H&Es.
When you do see stuff like this, consider the tissue trauma on the front end before it even got to the stainer could be causing your problem.
Poor Deparaffinization
In this slide you can see we have some irregular staining. We have some light pink here at the bottom, darker pink toward the top. This is a sign that your slide has not been appropriately deparaffinized. What can cause it? Well if your reagents are really dirty, your solvents, maybe you've been using them a lot and you haven't had a chance to refresh them. Maybe you don't have enough time in your solvent.
I prefer to keep mine in around two minutes and I have two changes of xylene and that works really nicely for getting out all of my paraffin, but if you're finding that that's not working for you, there's no harm in adding a third xylene if you want to.
I just try to minimize the amount of waste on my instrument and that's part of the way that I do that by having my two steps. Keep in mind if you're not drying your slides long enough before you stain them and you put them on there, the water is going to prevent the xylene from getting to that paraffin. The best way to prevent this from happening is to change your reagents regularly, and of course, make sure your slides are nice and dry before you put them on the stainer.
Poor Dehydration
In this slide, we can see there's some excess water left behind after we've gone through our dehydration steps on the way to cover slipping. And you can see I have an arrow pointing toward it here in the photo. But you can see there's water in different spots. What could cause that? If your laboratory is very humid, you can get some that ambient humidity into your xylenes. Of course, the other thing is if you're not changing your xylenes often enough, you can have water carry over from when it leaves eosins to the 95s, to the one hundreds. You'll start to get some water going across that. So that's why we do have recommended changes for your reagents.
The biggest way to reduce this problem is to make sure that your reagents are changed regularly. We want to make sure that we don't have any water in anything. If your lab feels like it's very humid, you can always purchase a hygrometer which will tell you what your room humidity is. Most staining equipment doesn't have a tight range for humid conditions, so you're generally going to be able to have quite a bit of leeway, but if you want to just track your humidity in your lab, that's one way to do that. and they'll certainly help prevent issues like this one. If there's water in your sample, you will start to see overtime when you put your slides in storage, you'll see a pink cast shifting across the side. That's the eosin coming out of the tissue. It’s kind of neat to see, but it also makes me sad when I see it.
Over Soaking Slides
We've all had those days where the tissue comes off the processor, we go to embed it, and we know it's going to be a rough day because it's super dry and crunchy. To accommodate that, oftentimes, we'll soak. Now I prefer my processing to be amazing so that I don't have to soak anything. You don't always get what you want, right? So that said, if you are having to soak your samples, you want to do it and be thoughtful about it. Now I can't say don't soak it longer than 5 minutes because that's going to vary depending on how dry your sample is.
If you over soak and unfortunately I do see this quite often, you can actually get some artifacts. Notice on these nuclei here, this is actually colon, and you notice how we have no nuclear detail at all. They look kind of cloudy and kind of slow.
When you are rehydrating on your, when you're soaking, when you're getting ready to cut them, unfortunately, it will create these types of artifacts which can cause you to lose the nuclear detail that can be so critical to diagnosis.
Prostate cancer is a great example of that because it's not known for being extremely hyperchromatic. When you do lose that nuclear salt and pepper chromatin that we would expect to see with this swelling and we lose that detail that can oftentimes negatively impact how we're doing our diagnostics.
Troubleshooting
Most of the common H&E related artifacts are very simply corrected. First of all, you always want to use quality reagents, so make sure your stains are good quality, your ancillaries, your alcohols, and xylenes. Those are all good quality and periodically test your water. You'd be surprised how much heavy rainfall or heavy snowfall can stir up the groundwater and give you wide variations in your tap water.
Filter your stains as needed to avoid floaters. If you have a lot of staining and processing of dry samples, floaters are always a risk. It's always a great idea to filter your stains just to make sure that you do remove any excess tissue or excess particulate that can happen in some lower quality hematoxylins. You want to filter those to get that out so you don't see that on your slides.
Cover your reagent containers if you're not using them. If you're going home for the evening, you want to cover those. You don't want them to be evaporating. You don't want them to be negatively impacted by your laboratory ambient environment. You can always have a hygrometer on hand to monitor humidity. They're very inexpensive and they're easy to get your hands on. But they're a helpful tool.
Maintain your instruments. I can't stress that enough. Doing good maintenance on them. Having your annual PMs. Those things are so critical to keeping all these things running smoothly for you.
Reach out to your vendor and get some refresher training for your staff. It's really interesting some of the places that I visit, I do have team members that don't get to spend as much time with the instruments, and then of course there's a day when all of the other key users are off and they have to go and use their instrument and try to figure out how to troubleshoot it when they may have touched it once or twice throughout a three month period. It's always good to give refresher training for your staff.
Depending on your locality, certification does require so many continuing education credits every year, so it's also a great opportunity to refresh your staff with their instruments. Also, the basics of H&E and to get them those continuing education credits to maintain certification.
Staining Recap – The Do’s
Always run a QC slide. Make sure everything's looking good. If you change out your hematoxylin, go ahead and run another QC slide. We want to make sure that that hematoxylin is performing to the expectations of your team.
If you change your ancillary reagents and you want to change out your whole instrument at once, run. If you see slide to make sure it is all looking good, but you should always run one before your first rack of tissues in the morning just to make sure everything's looking good.
Make sure that you have good wash water on your instrument. This one is so important. Make sure that your pH is where you needed to be and that you have good water pressure. Low pressure can make your slide rinse is ineffective or less effective than they otherwise would be.
Do select a protocol that's going to make sense for your slide reviewer. Make sure that you're meeting their expectations. It's going to make your life so much easier. Always use quality reagents, and of course filter your stains to reduce particulate and floaters.
Staining Recap – The Don’ts
Do not rush your staining times. There is nothing worse than trying to push something through and then having to redo it again because there was water in the xylene. The Hematoxylin isn't dark enough. Always take your time. It will save you time in the big picture.
Don't overuse your reagents. I know that it might seem like you're going to be saving a lot of money if you get just a few more slides but always try to follow the manufacturer’s recommendations for throughput. If you try to push it, it often can come back, and your slides will not look as good as you wanted to.
I usually discourage folks from using recycled reagents only because most folks don't test those reagents for purity. If you're doing your ethanol on a recycler and you're not making sure that you're getting 98 to 100% purity, you can be adding water to your xylenes. Remember on your dehydration step, you're going from a graded alcohol to a pure alcohol, to a solvent. If that pure alcohol is coming off your recycler and you think it's pure but it's not, now you're adding other contaminants into your xylenes. That's going to impede your coloration and your cover slipping.
Never neglect your staff. Make sure that they have good training, and you do annual reviews for competency on using your equipment. Very, very important. It's amazing, especially as hectic as it can be in the laboratory. If we don't get those refreshers, sometimes maintenance kind of goes to the wayside a little bit. We want to make sure that not only is everyone comfortable, but your instrument is given the love it deserves.
The Bottom Line
A good H&E is going to keep your slide reviewers happy and it's going to make sure they have the best possible foundation for diagnosis. Whenever you're working on your H&E’s, you always want to make sure that your colors look good and your slide reviewers are getting exactly what they need. There's always a patient at the end of whatever it is you're doing, so we do want to make sure that those foundations are as optimal as they possibly can be.
One of the key takeaways is that your stain is only going to be as good as your processing. If you're finding that you can't achieve what you're trying to do with your H&E, look at your tissue processing and make sure that it's as optimized as possible. You don't want to be having to soak samples for a long period of time. There's nothing worse than cutting into a piece of fatty tissue, laying it on your water bath and watching it explode because the center of that tissue hasn't been appropriately infiltrated.
Keep these things in mind, and you're going to have the best possible H&E experience in your slide. Reviewers will be happy with you.
Thank you for your attention today. I really appreciate you guys joining our webinar. If you have any questions, please feel free to share them. Now we'd like to open it up for any thoughts and comments that you might have.
About the presenter

Cindy Sampias is a board certified Cyto- and Histo-technologist. With more than 25 years of experience, she is a guest speaker at histology and cytology meetings around the country. She is a technical author for Media Lab, publishing a variety of technical courses and sharing best practices in histology.
Related Content
Leica Biosystems content is subject to the Leica Biosystems website terms of use, available at: Legal Notice. The content, including webinars, training presentations and related materials is intended to provide general information regarding particular subjects of interest to health care professionals and is not intended to be, and should not be construed as, medical, regulatory or legal advice. The views and opinions expressed in any third-party content reflect the personal views and opinions of the speaker(s)/author(s) and do not necessarily represent or reflect the views or opinions of Leica Biosystems, its employees or agents. Any links contained in the content which provides access to third party resources or content is provided for convenience only.
For the use of any product, the applicable product documentation, including information guides, inserts and operation manuals should be consulted.
Copyright © 2025 Leica Biosystems division of Leica Microsystems, Inc. and its Leica Biosystems affiliates. All rights reserved. LEICA and the Leica Logo are registered trademarks of Leica Microsystems IR GmbH.