Decalcification: What You Need To Know
The content of this webinar will encompass detailed technical descriptions of novel and state-of-the art methods to decalcify tissue samples that will be embedded in paraffin or for frozen sectioning for molecular and nucleic acid analysis for basic research purposes. Procedures to be discussed include EDTA, Formic Acid, and rapid decalcifying, with discussion of key technical considerations and basic chemistry in each case. Troubleshooting and discussion of approaches to surface decalcify already embedded and cut tissues will also be discussed.
학습 목표
- Review the various decalcification methods.
- Identify the appropriate decalcification method for your sample.
- Define the appropriate time needed for decalcification.
웨비나 전사
Decalcification: What You Need To Know
I’d like to get started today and talk to you about decalcification and what you need to know. So the learning objectives for today is to understand the different decalcification methods, to choose the appropriate decalcification method for your sample, determine the appropriate time needed for your decalcification, and review the chemical process of decalcification and how it works. Most of us already know that decalcification is the term used for removing mineral from bones or other calcified tissue, such as cartilage. This allows for proper press processing, and sectioning of specimens to be used for histological analysis.
Different types of Decalcification
There are different kinds of decalcification methods used in paraffin, and embedded formalin fixed samples. You can decalcify with acids, such as formic acid, hydrochloric acid, and nitric acid. And there is chelators, which are EDTA, tetra-sodium at various concentrations with varying pHs. Acids can vary. Some can be very strong and harsh, such as hydrochloric or nitric acid. At concentrations used up to 10%, they are used for rapid decalcification. These are really quick. You can also buy rapid decalcifying agents that are available commercially. I know many labs make them but I also know labs that purchase them because it’s easier.
Formic Acid
Formic acid is the most commonly used acid decalcifying agent. It varies from 5 to 20% formic acid, and can be and can be used in house or from an 88% stock formic acid. Formic acid is available commercially. Immunocal from Stat Labs is one that is commonly used. It’s the 5% formic acid concentration. Immunocal is very gentle but is also quick to calcify your tissue. And it’s a great low percentage to use, concentration. So when we’re talking about decalcification methods, I mentioned some acids.
EDTA
Now I’m going to go on and talk about chelators. A chelator, such as EDTA, tetra sodium at various concentrations and varying pH is, EDTA tetra sodium, a chelating agent, remove calcium’s, magnesium, and iron from bone, and calcified cartilage. EDTA takes longer to decalcifying compared to acid decalcifying agents. However, it’s much gentler on the tissue. In our lab, that is the standard go to. We use EDTA. Actually, we don’t even provide formic acid anymore.
When we do EDTA, we use two different variations. One is the web g method, and that is quicker than a standard 14% EDTA. Both of those recipes are included at the end of this slide show. EDTA, although it takes longer, you have to pay very, very close attention to it because of it taking longer can have a bad effect on the proteoglycan staining by removing the proteoglycans from the extracellular matrix of cartilage and bone. Now if you’re doing a stain and you want to quantify that, if you’ve over decalcified your sample and affected the proteoglycans, how will you measure that if the samples are going to vary?
Grossing
So grossing is a critical step in decalcifying process. Samples should be grossed down to the minimal size. Larger samples take longer to decalcify, obviously, which can damage cell, and tissue morphology. So we actually, right now in our lab, have samples coming in from a surgeon but there cadaver shoulder rotators, and rotator cuffs, and want the humorous, and rotator cuffs. So what we’re doing is taking the larger is taking a larger section of these samples, starting to decalcify them for one week, and then grossing them so that they— for another week and they are easy to handle. And we find that we aren’t damaging the tissue. If a sample is not grossed properly they will not fix well, which means they won’t decalcify well. If they don’t decalcify well, they’re not process well. They won’t cut well and it’s just a downward spiral, the domino effect. If things are grossed in the beginning formerly, the whole process is going to be terrible.
In our lab, our main focus is animal research. We do a lot of balance work. We also do some rat. Larger specimens come in, too. But mainly, our bread and butter is the mouse hind limb. So what we grossed them, we have to remove all the skin, the fur, and the muscle tissue, except for that which is immediately around the joint because we are the center for muscle skeletal research within the department of orthopedics. We are very interested in the joints, whether it be arthritis or some sort of manipulation. So we need to leave extra tissue around the joint to support it. And we cut off both, and the distal and proximal, and of the femur and tibia in order to allow the fixation to penetrate three days. We do a 72-hour fix and then we will do a good rinse. Here is an example of a grossed hind limb with the extra tissue around the joint. And they will cut the proximal and distal ends off the bone and remove the tibia. But this is just the picture I had where I wanted to show the expert tissue around the joint of the hind limb.
Here is a femur fracture, where you can see at both ends of the femur there is some extra tissue and muscle. That’s because it’s necessary in order to hold the femur fracture together, so it won’t break when we're embedding or cutting sectioning the sample. Other than that, that’s about the biggest femur I’m going to get in my lab. It makes it very easy for us to decalcify where I know in many clinical labs, you guys don’t have that luxury. But we do. So as I said, fixation is a critical step in the decalcification process. If samples aren’t fixed well, they also won’t decalcify well.
Fixation
We fix all our samples and 10% neutral buffered formalin. Sometimes there’s, very minimally, though, we use fresh 4% paraformaldehyde according to a timetable that will be posted. Postnatal and adult mouse limbs we fix for three days, like I mentioned, the 72 hours in NBF or 4%, paraformaldehyde. You can do 4⁰ or you can do temperature. It really doesn’t matter. I do, however, switch out the NBF daily, as well as the paraformaldehyde. Postnatal and adult spines fix for three day or 72 hours in 10% NBF all 4% paraformaldehyde at 4⁰ or, like I said, temperature. It’s really up to you. As I said, I really suggest that you change your NBF daily and definitely use fresh paraformaldehyde.
When you’re using calcified agent or anything, whether you’re fixing or decalcifying, you should have a 22 1% ratio solution according to your sample size in order for better infiltration. We prefer to place our samples and containers with magnetic stir bars and stir lightly. Or, we put them on a rocker so that they agitate. I have found this to be critical. We do this with all of our samples we don’t just them on a shelf to see what will happen. They rock and agitate. It speeds up the process of decalcification. Here’s a picture of the—some of you may recognize these. These are old microwave processing vessels that are on the stir bars. We put our cassettes in the racks with our decalcifying a solution and let them stir for generally about a week, seven days for the hind limbs. We change our solution every five days. And it’s very important with all of your solutions and histology, which you all know, that you change them regularly and keep them fresh. Post fixation is something that I’m big on. I post fix many of our samples after they’ve been decalcified. In our hands, it improves the cell morphology and yields crisper staining results. I have seen it. I’ve had people say, “Well, we don’t think that this is the case.” And you know, I don’t have any real evidence, other than in our hands, we have seen that makes a difference.
And it’s also—sometimes , as we are a fee for service core and sometimes the samples that come to us have already been decalcified. And so, somebody will say, “This is fixed. It’s been fixed for three days. We decalcified it. Now, we just want you to process it and vet it and section it.” Well, we only hope that what they’re telling us on this truth that yes, we did fix our samples for three days and 10% neutral buffered formalin. We changed formalin daily. And now we used EDTA for seven days for two weeks. But that’s not always the case. So I tried very hard, doesn’t always work. But I asked that people bring samples to us right out of fix and then we go from there in the process forward until we cut and stain at the end. That’s not always an option. So if something comes to me, even if they say we decalcified it, it’s this, it’s that, I still will put it in 10% NBF for a post fix station step.
And for larger samples focusing on joint injury or manipulations, muscle and connective tissue are not completely removed. After decalcification, the samples are post fixed in 10% NBF using various times, depending on size and rate 10% NBF penetrates tissue. Obviously, decalcification is going to take longer with a larger sample, as well as fixation is going to take longer with a larger sample. 10% NBF penetrates tissue rapidly but fixes slowly, about 1 mm/h. So that needs to sink in. Most of us already know this, though, that it penetrates tissue rapidly but fixes slowly. Therefore, the center of the ball may not be completely fixed. And see that a lot on stuff that has come in to us, as I said, that, oh, we fix this and we’ve already decalcified it. If it’s not, we have to go by what they say. When we’re cutting and staining at the end, we can tell that it wasn’t a three day fix or the standard time of decalcification in which we do.
Rinsing
You should thoroughly rinse EDTA out your entire sample. We placed ours under running water for several hours. And as long as your samples have been fixed proper, this isn’t a problem. Nothing swells, but they have to be fixed a good amount of time in order to do this process of running water. And we do. We run a rubber hose right off our spigot into our sample container and just let the water flow for probably at least three hours with samples before processing. What rinse it out tissue after acid decalcifying neutralizers must be used. So if you’re just rinsing EDTA out of something, a chelator you’re fine. You don’t need to follow up by a neutralizer. But if you use an acid, you have to neutralize the sample by bringing the pH back down. So that’s important. You can’t just run your sample underwater and hope that it’s going to work because the pH has been affected, which is going to affect your stain. It’s going to affect any immunohistochemistry or enzymatic staining that you hope to do in the future.
Subject to the amount of salt containing solutions that bone is subjected to, it must be rinsed thoroughly before processing. So the salts start maybe in grossing in PBS and then, in fixing in 10% neutral buffered formalin. And then, you’re going to your decalcifying agent. If you used EDTA, there’s a lot of salt. And if you do not rinse your sample out, when you change your processor at the end of however many runs your lab does, when you’re dumping the ethanol, you’re going to see that there’s a lot of salt going down the drain. Our processor starts in 70% ethanol. We don’t even have neutral buffered formalin on our processor. But we still see the salt. So if you have NBF as the first station of your process as the first station of your processor, you’ll see more salt but however choose to do in your lab, if it works for you, keep it that way. Acid decalcifying agent must be changed daily. That’s because they break down quicker than the EDTAs or the chelators. Acid decalcifying agents must be checked often, as the rate they decalcify varies.
EDTA
EDTA is not needed to be changed daily. Like I said, we change every five days, and most of the time, we do a seven day decal, so will do a Monday or a Tuesday and a Friday change for our samples. So the EDTA that we use is a 14% EDTA tetra sodium with a pH of 7.32 to 7.6. This is the Kimmel-Jee protocol I was talking about. We walked that in our lab. We use our regular 14% EDTA with the same pH that we have so that the web G is brought to pH with using glacial acetic acid. I have to think about that. It smells like vinegar every time we use it. And that is a quicker EDTA. If it’s still 14%, if the pH is 7.3 to 7.6, but it is a much quicker EDTA. It can decalcify samples in seven days, whereas another 14% EDTA tetra sodium with the same pH we use in this lab we bring down with hydrochloric acid to pH. It takes up to two weeks. So I’m a huge fan of the Kimmel-Jee and that, like I said, that’s going to be a protocol that you’ll find at the end of this slideshow.
When you’re going to decalcify your sample, you really have to think about your end result. What do I want to do with that sample? Am I going to want to do a safranin O stain because I’m going to want to look at the cartilage. Or am I just going to do these samples and—I’ll just do regular H and E, and then I’m going to do immunohistochemistry at the end. Well, you need to know exactly what it is you are going to do because if you use acid decalcifying agents, they are known to be fast. And they do. They remove fast and effective forms of removing calcium. They can be really harsh. Furthermore, they can destroy enzymes. They could destroy cell morphology. Acid decalcifying agents have a low pH that can interfere with enzymes, antigens, and stain quality, as I already said. I said that prior. Formic acid is a lower grade acid. It allows for good cellular, detail and works well with the common skeletal stains that we use. So you can use formic acid if you’re doing Alcian blue, hematoxylin, and Orange G stain, but like I said, we actually say in the last six months, we have used formic acid in our lab at all. We are strictly EDTA decalcifying lab.
So there’s rapid decalcifying agent may be necessary in clinical labs for quick results. In our research lab, we don’t have to have quick results. Obviously, we want to bring stuff in and turn that around to get it out as soon as we can. But in clinical labs, if that was your bone and it was sitting in EDTA for 2 weeks on a stir plate, that’s kind of disturbing. The rapid decalcifying agents, they are very harsh on samples. And they decrease cell-preservation and they also make so that the staining quality is poor. If you do an immunohistochemistry again, this could be a big problem. And which decalcifying agents work best for IHC immunohistochemistry? Well, some people will so you buffered formic acid with sodium citrate or the 14% EDTA? Well, what I will tell you is, whatever decalcifying agents you use in your lab, you better make sure that you do trial run on the immunohistochemistry on your antibodies and have some extra slides before you do the whole deal so you haven’t wasted reagent and time. We do lots of preliminary work here.
So again, we are still talking about how you choose your decalcifying agent wisely. When performing enzymatic stains, such as tartrate resistant acid phosphatase TRAP, we do a lot of TRAP in our lab, and beta-galactoside BETA-GAL, you should use EDTA just because if you use formic acid or any of the other acids, there’s going to be a lot of missing stain. It may not even stain at all. You won’t get any of the enzymes. Decalcifying at 4° for IHC or immunofluorescence to preserve antigens and fluorescence, that’s very important. And if you’re even doing laser capture microdissection, you’re going to want to make sure that either your decalcifying agent was purchased from a sterile environment or made in a sterile environment with depth sea water, autoclaved, also. It all goes back to knowing exactly what you want to see at the end.
So keeping decalcifying time to a minimum is necessary. It’s very important for lots of reasons, because we don’t want to have all of our samples sitting here and people waiting and waiting for them. We also know that the longer a sample six in a solution, the enzymes will die. They're pH and temperature sensitive. Antigen loss, preserving antigens is essential for immunohistochemistry and antigen retrieval. So again, should I keep this in 4⁰ and change the solution often or keep it to a minimal amount of time for decalcifying? And the longer that your sample sits and a decalcifying agent, the worst results you’ll have proteoglycans. So cell loss and poor cell morphology are going to be critical problems, to, if you’re samples have sat in a calcified agent for too long.
So keeping the decalcifying time to a minimum is necessary to prevent poor infiltration during processing, which will cause terrible sections. And if terrible sections is an issue surface decalcifying may be an option. I don’t even like to bring surface decalcifying up. But accidents happen, whether it is somebody bringing samples to you and saying, “I’d like to submit these samples to your core to have you process and embed and cut them. And I’ve already done the fixing and decalcifying. All you have to do is process.” Well, we hear that quite often. As a fee for service, people can bring in things that they’ve started along the way. And it saves them money. So I understand that. But it doesn’t save them money if we get to the end and they have made their EDTA and their lab, went and bought it, and that’s okay. You can buy it. You could make your own in your own lab. But you have to make sure that the pH and the way that it was pH-ed with what chemical in the same way that we do. Otherwise, when we go to cut these samples, we find that we are cutting into something that is just horrible. It scratches and there is still a whole bunch of minerals left in the sample.
Surface Decalcification
So how do you surface decal? Well I don’t know how you do it, but when we do it, we put a little bit of ammonia hydroxide in a top of a petri dish or a bottom of a petri dish. And then, we let it sit, not long, and I don’t have an approximate time to tell you. But you're going to have to pay close, close attention to your sample in your lab by yourself and figure that out. But we will put a sample on ammonium hydroxide a little bit for maybe 30 seconds is where we would start. And then, you have to rinse the sample off with water and then go ahead and cut it because if you aren’t rinsing the ammonium hydroxide off your sample, you're dropping the pH substantially. And then your stains are going to be off because you’re taking your sections from this ammonium hydroxide to water to the Microtel. But if you don’t rinse it well enough, you’re also contaminating your water bath, putting it on the slides.
When you send your slides to be stained, you’re going to see a whole lot of variables in the slides in the stains because of the surface decal. And like I said, I’m not a big fan but sometimes, that’s the only thing you can do. We’ve actually had samples come to us where people have not decalcified them at all. And somehow, that has come through the paperwork that yes, yes, we decalcified. So okay, they decalcified. We rinse out the samples and we’ll process them. And, when we go to cut them, oh, these samples haven’t been decalcified at all. Then, you have to obviously back them up, go through a reverse processing step, put them into decalcification agents and hope that everything will be okay. Obviously, reprocessing isn’t something you want to do, either. But it can be done. And if that’s how you have to save your samples, that’s what you have to do.
So there’s a weight testing that can be done on the whole with a milligram balance. This is an accurate and quick decalcifying endpoint test. Weight and reference sample weight prior to adding a decalcifying agent—so you way your sample and then, when the sample gains weight, they are decalcified. When calcium has been removed from the sample, it will take in water and increase in weight. Weigh EDTA samples daily and acids samples every five hours because they are so much quicker. Now is it important to do a specific task sometimes? And honestly, I was taught to put a mouse hind limb between my daughter and forefinger and to bend it. And it was spongy and bad, then it was done decalcifying. That’s great, but how do I know that my little bend test feels the same in every specimen in every strain of mouse or every age points? That became a problem when we started to say all right, we have to make sure that things are standardized in here, and how can we do this? What test should we do to make sure that everything is decalcified properly? This weigh test is easy. I mean, anybody can do that. .X-ray will confirm if calcium remains in the bone or not. We have that in our lab, too. Not all labs have that luxury.
A chemical test using ammonium oxalate will determine decalcification endpoints of acid. If calcium is present a precipitate of calcium oxalate will form, indicating longer decalcification is required. Mechanical testing can be done on the bone by bending carefully to see flexibility. This is what I mentioned. And this is how we used to do it in our lab. But I don’t recommend it. It can damage the bone and it’s not accurate. It varies between samples and it varies between technicians. It varies between people. You can’t keep that standard and in science and research, we have to be able to replicate everything that we’ve done. So obviously, that’s not a good idea to try.
Take Home Messages
So the take-home message here is that strong mineral acids, such as hydrochloric or nitric acid at concentrations up to 10% are used for rapid decalcification. They remove calcium quickly and are considered harsh on tissue morphology. Formic acid and organic acid is commonly used and gentle on tissues. As I said, formic acid can be made in your lab or it’s also available commercially. EDTA is a chelating agent that also you can buy that commercially or make it in your lab at varying concentration, so varying pHs. I’ve seen percent and 8% all the way up to 20% EDTA. Use a standard 14% EDTA in our lab. Large tissue needs to be post-fixed to allow proper dehydration infiltration during processing. I’m going to say all tissue in my lab, but in your lab, you may only want to do the large tissue. Or maybe you want to do any. I just found that in our hands, post-fixation is of great help.
If tissue is not grossed thoroughly, fix will not penetrate effectively. And you can see I have a picture of those lovely dominoes on this slide. If tissue isn’t grossed well, if the ends of the bone aren’t cut off, the fix won’t penetrate. If you leave skin on, say mouse tail because you’ve done something to the mouse tail and you're worried that if you fractured it, say, and you’re worried that if you remove the skin on an early injury, it won’t hold and maybe the callous will break. That’s going to be a real bear to fix, decalcified, and—it’s just going to be a whole bear to do anything with, especially when it comes to cutting if you’ve left the skin on.
Decalcifying will not be adequate if samples aren’t grossed and fixed, as I said. If something isn’t grossed wonderfully but fixed for a short period of time, you’re also going to have to same problem with your decalcifying aged. It’s not going to work right. And your samples are not going to cut right. And it’s just going to be so frustrating for the technician that’s in the Microtome. That’s why we post fixed, as I said all of our samples. And it allows the proper dehydration infiltration during processing. If any of these steps aren’t right or the steps are done right, then you have the domino effect.
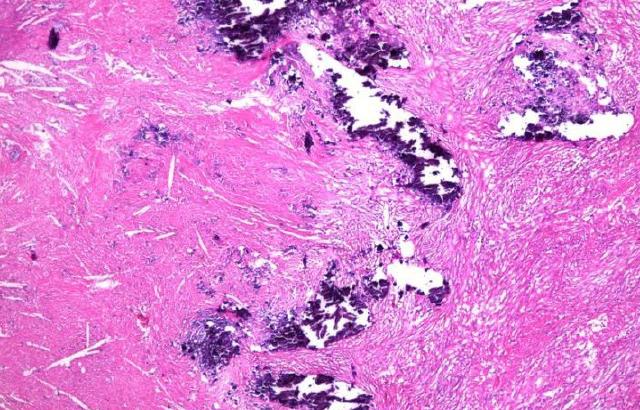
Right here is a stain done on a mouse hind limb. It’s the hematoxylin and eosin on the top. And you can see that the arrows on the top where the hematoxylin and eosin is pointing to just the articular cartilage. Below, we have Alcian blue, hematoxylin, Orange G. The top and the bottom are both done, actually, with formic acid as the decalcifying agent. And that would be a five day decalcifying process. This is Alcian blue Orange G done with, decalcified with 14% EDTA, pHed with glacial acetic acid to 7.36. And I think that that’s a pretty slide. Here is Safranin O Fast Green and Toluidine Blue Fast Green. Both of these, again, all these pictures are mouse hind limbs and the articular cartilage is what we’re most interested in. And both of these samples were decalcified with EDTA.
References I would like to point out are on this slide. And my contact information is Sarah_Mack@urmc.rochester.edu. Please don’t hesitate if you have any questions. Please contact me. I’d be more than happy to help you. Thank you for attending. I’d like to remind everybody that one of my collaborators here at the University of Rochester, Loralee McMahon, will be giving a presentation in April. I hope you can attend and listen to her conference as well. If you have any questions, I’d be happy to answer them.
Q&A
First is, would you post fix a bone marrow core sample after calcification, the largest measuring 1.8 x 0.3 cm and smallest 0.2 x 0.2 cm? So 1.8 x 0.3 and 0.2 x 0.2?
MS. MACK: That I probably put would not post fix. In my hands, I wouldn’t. This is mainly for research and for mouse and, well animal tissue. As far as human bone marrow cores, I think that I would not post fix that.
How much weight should the specimen gain, a certain percentage of the original weight? That was around slide 29 or 30. I’m not sure exactly what that’s referring to but I think you do.
MS. MACK: that is just, if it starts gaining weight at all, any weight at all, as soon as it starts gaining weight, you’re going to notice. It’s not a certain percentage because all sample sizes vary in the amount of water that they’ll intake as weight will vary. When it starts gaining weight, it’s complete.
We are a research core and receive large pieces of human spine, 3” x 2” and by 1” inch thick. The investigator does the fixation and decalcification. Some samples are fine but others are awful. What can you recommend as the time for the fix and calcification?
MS. MACK: Okay, so that’s a tough one. But you did say research, correct?
RICK: Correct, research core.
MS. MACK: Okay, so in that case, we have the option. I don’t know if this is something that you can do, but I tell people that their samples must be able to fit into a mega cassette. In the beginning, I understand that’s not always an option. So in the beginning, once a sample is fixing, that might not be possible. So you would put it in a container where you could have a 1:20 ratio of - - formalin and then fix at least three days, especially these are very large samples and then, when it comes to decalcifying, this is where we decalcified for a week and then I say to my people, “Okay, you’ve given me this large femoral head. Now you need to cut it down and make it so decalcifies,” because the larger the sample, all is going to do is decalcify on the edge. In the center, it won’t be decalcified the same as it is on the edges. So I just make sure that the fix for three days. They decalcify for seven, then we gross, and we go from there. And you have to do a weight test to see exactly when it was completely decalcified. But that’s what we would do.
Do you have any experience with fish and decalcification?
MS. MACK: No, I do not. But if you would like to send me an email, my contact information is they are. I would be happy to try and help you find out about this and steer you in the right direction of someone you could speak to that could help you.
Could you add some more details oxalate ammonium, the oxalate ammonium test?
MS. MACK: That is in the handout, I believe. Well, it’s not a handout but, it is, it is one of the slides at the end of the presentation, which will be available to you. Not, email me and I’ll send that information to you. Just ask specifically for the oxalate test and I can send it to you.
Have you ever decalcify samples from human, from nonhuman primate? If so, how long do you need to decalcify? Is there a way to expedite this process?
MS. MACK: I am very sorry. I have not done anything with nonhuman primates. If you want to email me that question with your contact information, I can see if there’s anybody that is in the field that I know of that able to help you with that
How you decalcify teeth for sectioning?
MS. MACK: Depends on what kind of teeth they’re talking about. We did a study with dog teeth. And we decalcified them with formic acid very long time, I believe. I can’t remember exactly, but there are also books available through the National Society of Histotechnology that has some suggestions for decalcified time. That, again, it depends on exactly what kind of teeth, how long they would decalcify for, and even what process you would use. There are a lot of variables to that question.
What commercial EDTA solution you, well we don’t want to actually have product recommendations so let’s move to the next one. Have you ever used a fixative with EDTA in it?
MS. MACK: I actually have not. I do know that many people use that.
We are a research facility and use EDTA post fix with formal saline. We use the weight method as well. Unfortunately, we have bigger samples of rat pause and it takes longer, UP to eight weeks. We use lower concentration of EDTA in 5.5% we will try the 14%, as you recommended. Thanks again. Just more of a comment that a question, so.
MS. MACK: Well, that’s great. You’re welcome.
Is there any chemical methods test for the endpoint of decalcification with EDTA? We are working on whole adult zebrafish.
MS. MACK: There is. I didn’t put it in your handout. If you email me, I can send you information on the chemical endpoints for EDTA as well.
How can we explain the good results for IHC, the temperature 4° of C in EDTA and how long must it be for the bone marrow samples? If that’s not clear, we’ll just move on. You want me try that again?
MS. MACK: You can move on.
RICK: According to your presentation, for a mouse knee decalcification, the best protocol should be three days with fresh 4% PFA and 14 days with 14% EDTA glacial acetic acid with a pH of 7.3 to 7.6 Is that correct?
MS. MACK: No, we do, and I won’t say it’s the best. It’s the best in our hands, but it might not be in your hands. What we do in our lab is we do, on a mouse hind limb, as long as they are grossed right with the proximal and distal end of the hind limb cut off and you have to have some tissue remaining around the joint. If they are grossed well, like I said, a fix for three days in 10% neutral buffered formalin, changing the solution every day, then you can put just sample into a 14% EDTA pHed at 7.6 or 7.3 to 7.6 for about seven days, changing the solution every five days. You don’t want to do a 14 day decalcifying time in that solution.
Have you ever calcified cochlea? If so, what’s the best way to do this?
MS. MACK: I have not. I’m sorry. I have no idea.
Could you give us any more details about the oxalate ammonium test?
MS. MACK: If you email me, I’ll make sure that you get that protocol. It should be in the back of the slideshow here from Leica.
Our lab mostly works with bone metastasis samples and we are interested in genomic alterations. We usually use 14% EDTA but sometimes, that will not soften samples. And we switched to 5% nitric acid. Which decalcification agent do you recommend for genomic studies?
MS. MACK: That’s a tricky question to answer. I think that EDTA is great. But if you need to get your samples in and out quicker for larger samples, then you’re going to want to use an acid based decalcifying agent. And for genomic - - you don’t want something that’s going to sit around and destroy your sample. So I’m not sure. We don’t do that work, so all I would say is that you’re going to want something that is going to allow your sample to come in and out quicker.
What are the important points to remember when using infant samples for the decalcification process?
MS. MACK: Well, the most important process to decalcifying anything is just as, you need to know what you want to see in the end and that’s a tricky question, too, what your end result is going to be. I see a special stain. It depends. I really don’t know exactly how to answer that question.
발표자 소개

Sarah A. Mack has over a decade of experience as a histotechnician, with a main focus on preparation, processing and analysis of both calcified and soft tissues of the musculoskeletal system. In addition to providing consulting, advice and assistance to clients of the HBMI Core, Sarah serves as its Manager, supervising all histology-based projects within the Center of Musculoskeletal Research. Sarah supervises the generation of musculoskeletal tissue biorepositories, and oversees the creation and maintenance of reagent stocks and standard protocols. She provides hands-on assistance in the preparation of histological tissues, including decalcification, automated paraffin processing, orientation before embedding and sectioning of paraffin and frozen tissue.
Sarah currently serves as Chair of the Hard Tissue Committee for the National Society of Histotechnology and as President of the New York State Histotechnological Society. She has been an active member in both societies for more than 15 years, providing information and knowledge to histologists that work in both scientific and clinical lab settings.
Related Content
라이카 바이오시스템즈 Knowledge Pathway 콘텐츠는 에서 이용할 수 있는 라이카 바이오시스템즈 웹사이트 이용 약관의 적용을 받습니다. 법적고지. 라이카 바이오시스템즈 웨비나, 교육 프레젠테이션 및 관련 자료는 특별 주제 관련 일반 정보를 제공하지만 의료, 규정 또는 법률 상담으로 제공되지 않으며 해석되어서는 안 됩니다. 관점과 의견은 발표자/저자의 개인 관점과 의견이며 라이카 바이오시스템즈, 그 직원 또는 대행사의 관점이나 의견을 나타내거나 반영하지 않습니다. 제3자 자원 또는 콘텐츠에 대한 액세스를 제공하는 콘텐츠에 포함된 모든 링크는 오직 편의를 위해 제공됩니다.
모든 제품 사용에 다양한 제품 및 장치의 제품 정보 가이드, 부속 문서 및 작동 설명서를 참조해야 합니다.
Copyright © 2024 Leica Biosystems division of Leica Microsystems, Inc. and its Leica Biosystems affiliates. All rights reserved. LEICA and the Leica Logo are registered trademarks of Leica Microsystems IR GmbH.